Best AI SOAP Note Generator for Every Specialty: Psychiatry to Cardiology
.jpg&w=3840&q=75)
AI SOAP notes are transforming healthcare by solving one of its biggest problems: documentation overload. According to a study, physicians spend about 27% of their total workday creating and updating clinical notes. The American Medical Association reports that 62% of clinicians cite documentation as their top stressor.
AI SOAP notes automate this process using natural language processing and real-time transcription. It records patient interactions and generates structured, accurate notes instantly. They personalize documentation for each specialty, including psychiatry, pediatrics, cardiology, and more, unlike rigid EHR templates.
According to HealOS data and industry reports, the best AI SOAP note generator cuts charting time by up to 70%. It allows doctors to spend more time with patients instead of on paperwork. Let’s see how AI transforms documentation across specialties.
What Are AI SOAP Notes and Why They Matter in 2025?
AI SOAP notes simplify medical documentation for busy clinicians. SOAP stands for Subjective, Objective, Assessment, and Plan. The subjective part includes what the patient says. The objective covers test results and observations. The assessment outlines the diagnosis, and the plan lists treatments or follow-up steps.
Traditional dictation and EHR templates are slow and rigid. AI SOAP notes use natural language processing to listen, understand, and organize patient encounters in real time. They turn spoken notes into structured, accurate summaries instantly.
Modern systems like HealOS (formerly Scribehealth) use HIPAA-compliant AI scribes and real-time transcription to keep data secure and error-free. Doctors spend less time typing and more time caring for patients. This reduces burnout, improves accuracy, and makes every clinical workflow faster and smoother in 2025.
Learn BIRP vs SOAP Notes: Which Documentation Format is Right for Your Practice?
1. SOAP Notes for Psychiatry and Mental Health

Psychiatrists face one of the highest documentation burdens in healthcare. According to recent studies, psychiatrists spend 30–40% of their day writing notes for 45–60 minute sessions, increasing burnout risk. AI SOAP notes automate this process using real-time transcription and psychiatric language recognition. The system captures
- DSM-5 criteria
- Medication changes
- Therapy modalities like CBT or DBT
- Records Mental Status Examination (MSE) details such as affect, mood, and thought process
A 2025 study found psychiatrists saved up to 3 hours daily using AI scribes, while 78% of patients felt doctors were more attentive. Dr. Andrea Partida, DO, shared, “I can now maintain eye contact with patients instead of typing.”
These systems are fully HIPAA-compliant, protecting sensitive data while creating accurate, structured SOAP notes. Psychiatrists report better balance and deeper patient engagement thanks to AI-driven documentation. Here are the Best AI Scribes for Psychiatry in 2025.
2. AI SOAP Notes for Pediatrics and Children’s Healthcare

Pediatricians face unique documentation challenges. They record details from parents, caregivers, and children while tracking growth, milestones, and immunizations. A 2024 survey found 73% of pediatricians cited EHRs as a major burden.
AI SOAP notes simplify this, though:
- Multiple speaker identification (clinician, child, parent/caregiver)
- Growth chart documentation (height, weight, BMI percentiles)
- Developmental milestone tracking
- Vaccine schedule and immunization records
- Age-appropriate symptom descriptions
- Parent communication and education points
University of Waterloo researchers conducted groundbreaking research with the KidsAbility Centre for Child Development, examining 432 SOAP notes: AI tools generated SOAP notes with quality comparable to human-authored notes. An AI medical scribe is transforming pediatric care. Discover How AI Scribes Streamline Children's Clinic Workflows.
Dr. Emily Johnson, a New York pediatrician, said, “I spend more time talking to families instead of my screen.” These AI systems follow AAP guidelines, ensuring compliant and age-appropriate documentation.
3. AI SOAP Notes for Cardiologist
Cardiologists manage complex, data-heavy documentation daily. They spend about 10 hours weekly recording results from EKGs, echocardiograms, and stress tests. AI SOAP notes
- Real-time capture of cardiac symptoms and cardiovascular history
- Automatic documentation of diagnostic test results (EKG, echocardiogram, stress tests)
- Recognizes cardiology-specific terminology and suggests ICD-10 codes
- Auto-summarization of cardiac history, including chronic symptoms, family history, test results, and imaging
- Context awareness, pulling relevant data from past visits
- Integration of interventional procedures and catheterization reports
The AI identifies cardiac terms, summarizes imaging findings, and suggests ICD-10 codes like ischemic heart disease or arrhythmias. AI SOAP notes help cardiologists cut charting time by over 50%, ensuring complete, accurate records that support faster, safer cardiac care.
4. AI SOAP Notes for Neurologists

Neurology documentation is complex. It covers seizures, strokes, migraines, and movement disorders. AI SOAP notes handle this by
- Real-time capture of neurological examination components (cranial nerves, motor strength, sensation, reflexes, coordination, gait)
- Documentation of cognitive assessments and mental status examinations
- Detailed stroke assessments, including NIHSS scores
- Recognition of neurological terminology (hemiparesis, dysarthria, ataxia, nystagmus)
- Integration of imaging findings (CT, MRI, EEG results)
- Documentation of seizure descriptions and patterns
- Multilingual support for diverse patient populations
In a 2025 Neurology® study, 80% of neurologists reported faster reports and better accuracy. Average note completion dropped from days to minutes. Ambient AI tools even convert multilingual consultations, turning Russian, Spanish, or English speech into accurate SOAP notes.
AI SOAP notes now help neurologists document chronic and acute conditions with precision. It frees time for diagnostics and direct patient connection. Explore AI Scribe for Neurodivergent Therapists: Smart AI Tool for ADHD, Autism, and Mental Health Support.
5. AI SOAP Notes for Surgery

Surgeons rely on precise pre-op and post-op documentation. While intraoperative notes differ, AI SOAP notes streamline pre-surgical assessments and recovery tracking. AI SOAP notes provide
- Ambient intelligence capturing OR conversations and procedure details
- Automated operative note generation with procedure terminology
- Time-stamped surgical milestones and critical decision documentation
- Surgical case summaries for quality improvement and research
- Video-synchronized transcripts for training and review
- Integration of device and physiologic data
In high-volume practices, AI reduces prep and post-op note time by up to 60%, helping surgeons spend more time in the OR and less at a desk. AI SOAP notes are rapidly becoming essential across all specialties, bringing accuracy, efficiency, and human connection back to medicine.
6. AI SOAP Notes for Oncologist (Cancer Care)
Oncology requires extensive documentation of lab results, imaging, pathology, and treatment responses. Oncologists spend 5–7 hours daily in EHR, nearly 50% of their working hours tracking multi-drug regimens and tumor board updates.
How Oncologists Use AI SOAP Notes
- Real-time data synthesis combines labs, imaging, pathology, and treatment notes into one summary
- Automated SOAP notes achieve up to 95% accuracy with complex oncology terms
- Smart treatment summaries organize drug regimens, doses, and monitoring schedules
- Tumor board prep happens automatically with all key data in one place
- Cancer staging and genetic test results are added directly to the record
- Treatment response tracking monitors progress and disease changes in real time
- Automated pre-charting saves oncologists 2–3 hours of prep time daily
At Ackerman Cancer Center, AI reduced administrative work by 50% and improved care coordination by implementing HealOS (formerly Scribehealth) AI SOAP notes. According to them
“AI pre-charting has transformed our workflow. What used to take 2-3 hours of manual chart review now happens automatically before each patient arrives. Our oncologists can walk into appointments fully prepared without sacrificing their evenings to chart prep.”
7. AI SOAP Notes for Family Medicine and Primary Care
Primary care doctors juggle multiple problems per visit and often treat 20–30 patients daily. According to JAMA Network Open, family physicians spend 36 minutes per visit on EHR tasks. AI SOAP notes automate this process by capturing multi-condition encounters in real time.
- Acute visit documentation (URIs, injuries, infections)
- Chronic disease management (diabetes, hypertension, COPD)
- Preventive care and wellness visits
- Pediatric well-child visits with growth charts and immunizations
- Geriatric assessments with cognitive/functional status
- Multi-problem visit capture
These tools also improve documentation accuracy and boost clinician satisfaction by over 80%.
8. AI SOAP Notes for OB-GYN Specialists

OB-GYN clinicians balance complex documentation from prenatal visits to surgeries and postpartum care. They spend 2–3 hours daily charting fetal monitoring, lab results, and counseling notes.
How OB-GYN Clinicians Use AI SOAP Notes
- Real-time fetal monitoring integration (NST, biophysical profiles)
- Automated prenatal visit summaries with fundal height, fetal heart rate, and labs
- Labor progress documentation (P-chart graphs, cervical exams)
- Cesarean and operative note generation with surgical details and anesthesia records
- Gynecologic procedure notes (hysteroscopy, laparoscopy)
- Patient education handouts for prenatal care, breastfeeding, and contraception
- Integration with obstetric EHR modules for scheduling and registry reporting
- Alert systems for high-risk pregnancies (pre-eclampsia, gestational diabetes)
A 2025 multicenter study found that ambient AI scribes in L&D units cut charting time per delivery by 30%, automatically generated real-time partographs, and ensured 100% capture of medications and Apgar scores, improving accuracy and workflow efficiency.
9. AI SOAP Notes for Emergency Physicians

Emergency physicians face a relentless pace and heavy documentation demands. They manage 20–30 patients per shift across trauma, sepsis, cardiac, and psychiatric crises. Studies show doctors spend over 1.5 hours per 8-hour shift documenting time that delays care and fuels burnout.
How Emergency Physicians Use AI SOAP Notes
- Captures chief complaints and critical findings (ABCDEs, vital signs) in real time
- Automated triage notes populating ESI levels and initial interventions
- Fast documentation of lab orders, imaging studies, and consult requests
- Recognition of emergency terminology (PERC, Wells’ criteria, FAST exam)
- Structured discharge instructions for common presentations (UTI, asthma exacerbation)
- Integration with ED information systems (tracking boards, eMAR, CPOE)
- Time-stamped intervention logs for quality metrics (door-to-needle, door-to-balloon)
- Automated critical alerts for abnormal results and sepsis bundles
According to Dr. Sarah Li, MD – Emergency Physician:
“The AI scribe captures my entire trauma resuscitation, allowing me to focus on patient stabilization rather than typing. My notes are complete and accurate within minutes of the patient leaving the trauma bay.”
Read: Emergency Department AI Scribing: Capturing Critical Notes Under Pressure
What Challenges Do Different Specialties Face When Using AI SOAP Notes?
Different specialties face unique challenges with AI SOAP notes.
- Psychiatrists worry about capturing emotions and patient tone accurately.
- Pediatricians need AI to understand multiple speakers, like parents and children.
- Cardiologists handle complex data from tests and imaging that AI must interpret correctly.
- Neurologists need precise documentation for detailed exams and rare conditions.
- Surgeons require real-time accuracy during fast procedures.
- Oncologists manage long treatment histories that demand consistent updates.
- Family doctors handle many conditions per visit, so AI must stay organized.
- Emergency physicians need instant documentation during high-pressure, time-sensitive cases.
- OB-GYN providers require real-time fetal data capture and complete delivery records.
Each field needs AI SOAP notes that are secure, specialty-aware, and error-free. Now you See more patients and work fewer hours with AI Medical Scribe Breakthrough.
How HealOS (formerly ScribeHealth) Adapts AI SOAP Notes for Each Specialty
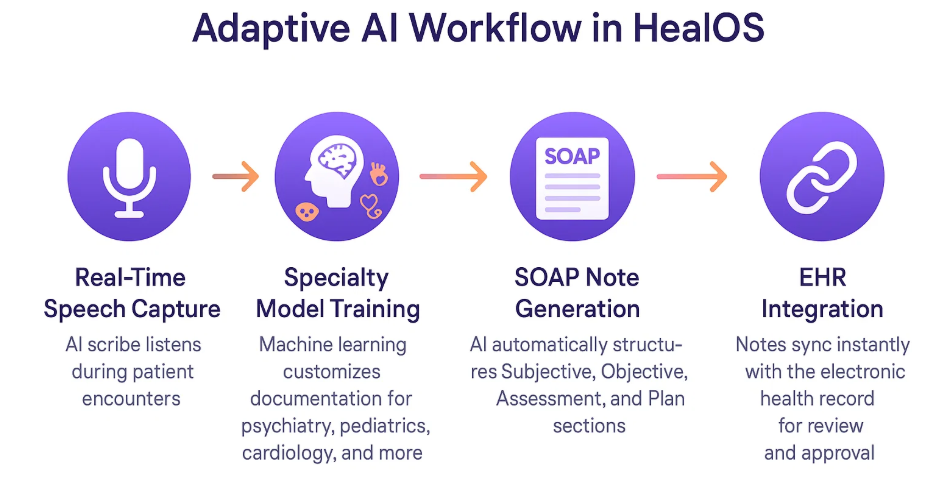
Every medical specialty has its own language, workflow, and documentation style. A psychiatrist’s note differs greatly from a cardiologist’s or a pediatrician’s. HealOS understands this diversity by creating specialty-specific AI documentation that mirrors how each clinician naturally works.
The platform uses machine learning to train models on specialty vocabularies, clinical abbreviations, and documentation patterns. For example, psychiatry models recognize DSM-5 criteria, while cardiology models interpret EKG terms and cardiac procedures. Pediatric modules capture milestones, caregiver input, and growth charts.
Each HealOS instance includes customizable templates and EHR integration, allowing automatic syncing of notes, vitals, and labs. Its ambient AI scribe listens passively, capturing clinical conversations without typing or prompts. Using machine learning clinical notes, HealOS adapts over time, improving accuracy with every encounter.
Ready to see how HealOS transforms medical documentation for your specialty? Book a Free Demo with HealOS (formerly ScribeHealth) best AI SOAP note generator. Discover how specialty-specific AI documentation can save you hours every day.
FAQs
What makes HealOS (formerly ScribeHealth) different from other AI medical scribe software?
HealOS is designed with specialty-specific AI documentation, meaning its models are trained on real clinical data from each medical field.
Is HealOS (formerly ScribeHealth) compliant with healthcare data privacy standards?
Yes. HealOS is HIPAA-compliant and uses end-to-end encryption to ensure complete patient data security and privacy.
Can HealOS (formerly ScribeHealth) integrate with my existing EHR system?
Absolutely. HealOS integrates seamlessly with major EHR platforms, automatically syncing SOAP notes, vitals, and labs into your existing workflow.